Digital technology offers huge opportunities for the health of people. Better registration, analysis and evaluation of medical procedures can result in better information, less risk, better health and greater quality of life for patients. Combining, analysing and applying large quantities of genetic and biomedical data can result in better diagnosis and in treatments which are tailored to individual patients rather than to large patient groups. All manner of smart technology can help to make hospital and home care more effective and efficient. At the same time, this care will have to remain collectively affordable.
Researchers introduce themselves:
Quality of life
Het is bekend dat geestelijke aandoeningen zoals depressie en angst veel voorkomen, een grote last voor de patiënt vormen en aanzienlijke kosten voor de maatschappij met zich meebrengen. Evidence-based farmacologische en psychotherapeutische preventie en behandelingen zoals cognitieve gedragstherapie zijn duur. Mijn groep stelt zich ten doel de toegankelijkheid, (kosten)effectiviteit en uitvoering van de preventie en behandeling van deze aandoeningen te verbeteren door gebruik van e-mental-health-technologieën. We hebben aangetoond dat therapie op basis van internet aanvaardbaar is voor patiënten en zorgverleners. Tevens is gebleken dat deze therapieën effectiever zijn dan niet ingrijpen en dat ze potentieel net zo effectief zijn als face-to-face behandelingen. Ons onderzoek duidt er echter ook op dat niet alle patiënten baat hebben bij therapie op basis van internet. De reden hiervoor is niet duidelijk. Wij willen de hiaten in de kennis aanvullen. Andere projecten betreffen de kosteneffectiviteit van gecombineerde behandelingen voor depressie en angst in de gespecialiseerde zorg, en de ontwikkeling en kosteneffectiviteit van kortdurende transdiagnostische internettherapie voor depressie en angst onder populaties van universiteitsstudenten. De resultaten van deze onderzoeksprojecten dragen bij aan de positie van Nederland als internationaal koploper op het gebied van e-mental-health.
Society continues to face great challenges regarding the health of its population, despite much research and innovation. For example, the incidence of cancer, age related osteoarthritis, continues to rise, which poses an unmet demand for better therapies that come at a lower cost. Our understanding of health is converging upon a personal molecular state of being, but how can we make medicine truly precise without a molecular understanding of human tissue? The translational research we perform in Maastricht targets to establish a comprehensive personal molecular state of health and disease.
 Innovative molecular imaging techniques generate profiles that reveal the local interaction and interplay of genes, proteins, lipids and metabolite in the context of human tissues. This patient specific diagnostic information is employed to make medicine precise, predictive and preventive. Cellular phenotyping allows us to address disease complexity and our inability to deal with this inconceivable complex interplay between different molecules, interconnected pathways and subtle environmental changes in diseased tissue. This molecular imaging research defines and delineates new clinical paths towards precision medicine.
Innovative molecular imaging techniques generate profiles that reveal the local interaction and interplay of genes, proteins, lipids and metabolite in the context of human tissues. This patient specific diagnostic information is employed to make medicine precise, predictive and preventive. Cellular phenotyping allows us to address disease complexity and our inability to deal with this inconceivable complex interplay between different molecules, interconnected pathways and subtle environmental changes in diseased tissue. This molecular imaging research defines and delineates new clinical paths towards precision medicine.Surgeons need to precisely know the nature of the tumor malignancy they are about to operate upon. However, it is sometimes still difficult to obtain the correct diagnosis using standard pathological screening. Data driven molecular imaging provides the opportunity to gain a more specific and objective diagnosis ahead of surgery based on diagnostic personalized imaging modalities amenable to potentially curative surgical resection. Clustering objective patient information provides more insight in diagnosis and therapeutic success and independent of personal interpretation. We bring together different levels of digitally available patient information with the personal molecular profiles of health and disease. This approach helps to ensure that patients receive optimal treatment or, perhaps even more importantly, prevent the use of unsuccessful or harmful treatments.
We are more and more aware of the fact that our current ideas about health don't hold true anymore. A new definition of health could be formulated as the ability to adapt and to self-manage in relation to physical, social and emotional challenges we face in life. This is hardly possible if the individual citizen has no direct ownership and understanding of their health-related data.
Changing position of the patient
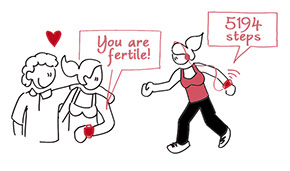
If citizens can manage their own health-related data, they will be better able to prevent illness, or to self-manage their illness if they do fall ill. We can empower them to do so with the help of adequate eHealth tools. Data ownership will even give them a say in any research performed with their health data.
Longitudinal view
Health data owned by patients can be stored and organized by collaborative data storage projects, such as Medical Delta's 'My data Our Health' initiative. This will lead to a life-long, or at least more long-term view on these data, which will over time improve our understanding of how diseases emerge, and how we can prevent them. We are increasingly aware that health is only for a small part related to healthcare, for the larger part it is related to hereditary, environmental, life-style and coincidental factors.
Integration of data
In order to use these integrated data we need to continuously validate their accuracy, reliability, and veracity with new forms of big data analytics. We also need to be able to integrate data from different sources, not all of them medical (e.g. wearables). This will enable us to identify groups of vulnerable people, such as the lonely elderly or women with high-risk pregnancies. We can develop more personalized forms of medicine, based on genetic background and adapted to individual needs and preferences. My research is to monitor real-world data and the outcome of diseases that really matter to patients, we can also manage the integrated costs and analyze the sustainability of our treatments (Value Based Health Care). In this way, we combine medical outcomes (cardiac function, levels of biomarkers etc.) with patient reported outcomes (quality of life, pain, depression, return to work etc.). Because we ask patients to report on their outcomes years after treatment we get a longitudinal view on their disease, as well as the effect of the treatment.
Privacy & cybersecurity
 To achieve all this, data should be findable and accessible under transparent conditions. We should also use terminology, classification and coding standards to ensure that data is interoperable and re-usable for other purposes than they were originally captured for. However, new privacy rules could make this difficult or even impossible. Security risks such as the hacking of personal data can also put a spanner in the works. To overcome this, collaboration between universities is more needed than ever.
To achieve all this, data should be findable and accessible under transparent conditions. We should also use terminology, classification and coding standards to ensure that data is interoperable and re-usable for other purposes than they were originally captured for. However, new privacy rules could make this difficult or even impossible. Security risks such as the hacking of personal data can also put a spanner in the works. To overcome this, collaboration between universities is more needed than ever.

